Endoscopy Balloon Placement Consent Form
Weight Management Unit Intra-Gastric Balloon by Upper Gastrointestinal Endoscopy (Gastroscopy) Assistance for Weight Loss
A. Interpreter/ Cultural needs
• The doctor has explained that you have the following condition: (Doctor to document in patient's own words).
• This condition requires the following procedure. (Doctor to document - include site and/or side where relevant to the procedure)
• An upper gastrointestinal (GI) endoscopy is where the doctor uses an instrument called an endoscope to look at the inside lining of your esophagus (food pipe), stomach and duodenum (first part of the small intestine). This is done to look at reasons why you may have swallowing problems, nausea, vomiting, reflux, bleeding, indigestion, abdominal pain or chest pain. This procedure may or may not require sedation anesthetic.
C. Risks of an upper gastrointestinal endoscopy +/- sedation.
There are risks and complications with this procedure. They include but are not limited to the following.
Common risks and complications include:
• Nausea and vomiting.
• Faintness or dizziness, especially when you start to move around.
• Headache.
• Pain, redness or bruising at the sedation injection site. (Usually in the hand or arm).
• Muscle aches and pains.
• Allergy to medications given at the time of the procedure.
Uncommon risks and complications include:
• About one person in every 1,000 will experience bleeding from the esophagus (food pipe), stomach and duodenum where a lesion or polyp was removed. This is usually minor and can usually be stopped through the endoscope. Rarely, surgery is needed to stop bleeding. Heart and lung problems such as heart attack or vomiting in the lungs cause pneumonia. Emergency treatment may be necessary.
• Damage to your teeth or jaw due to the presence of instruments in your mouth.
• An existing medical condition that you may have. gotten worse.
Rare risks and complications include:
• Missed polyps or growths.
• About one person in every 5,000 will accidentally get a hole (perforation) in the esophagus, stomach or duodenum. This can cause a leak of stomach contents into the abdomen. If a hole is made, you will be admitted to the hospital for further treatment which may include surgery.
• Your procedure may not be able to be finished due to problems inside your body o because of technical problems.
• Bacteremia (infection in the blood) This will need antibiotics.
• ‘Dead arm’ type feeling in any nerve, due to positioning with the procedure- usually temporary.
• Anaphylaxis (severe allergy) to medication given at the time of the procedure.
• Death as a result of complications to this procedure is rare.
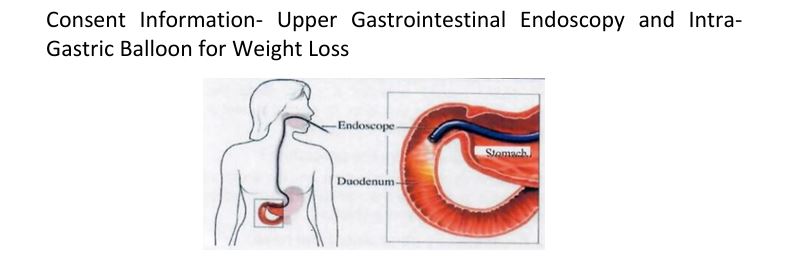
What is an Upper gastrointestinal endoscopy (Gastroscopy)?
An upper gastrointestinal (GI) endoscopy is where the doctor uses an instrument called an endoscope to look
at the Inside lining of your esophagus (food pipe), stomach and duodenum (first part of the small intestine). This is
done to look at reasons why you may have swallowing problems, nausea, vomiting,
reflux, bleeding, indigestion, abdominal pain or chest pain.
An endoscope is a long, thin, flexible tube with a small camera and light attached which allows the doctor to see the
pictures of the inside of your gut on a video screen. The scope bends so that the doctor can move it around the
curves of your gut. The scope also blows air into your stomach; this expands the folds of tissue in your stomach so
that the doctor sees the stomach lining better. As a result, you might feel some pressure,
bloating or cramping during the procedure.
This instrument can also be used to remove or burn growths or to take tissue biopsies. You will then lie on your left
side, and the doctor will pass the endoscope into your mouth and down your
Esophagus (food pipe), stomach and duodenum (first part of the small intestine). Your doctor will examine the lining
again as the endoscope is taken out. The endoscope does not cause problems with your breathing. You should plan
on 2 to 3 hours for waiting, preparation and recovery. The procedure itself usually takes anywhere from 10 to 15
minutes.
If the doctor sees anything unusual or wants to test for bacteria in the stomach, they may need to take a biopsy
(small pieces of tissue) for testing at Pathology.
This procedure may or may not require a sedation anesthetic.
Will there be a discomfort? Is any Anesthesia needed?
The procedure can be uncomfortable and to make the procedure more comfortable a sedative injection or a
light anesthetic can be given. If you prefer, it can be done without sedation. Before the procedure begins
the doctor:
• will put a drip into a vein in your hand or forearm. This is where the sedation or anesthetic is injected
and may spray your throat with a numbing agent that will help prevent gagging.
What is Sedation?
Sedation is the use of drugs that give you a ‘sleepy- like! feeling. It makes you feel very relaxed during a
procedure that may be otherwise unpleasant or Painful. You may remember some or little about what has
occurred during the procedure. Anesthesia is generally very safe but every anesthetic has a risk of side
effects and complications. Whilst these are usually temporary, some of them may cause long-term
problems.
The risk to you will depend on:
• personal factors, such as whether you smoke or are overweight,
• whether you have any other lines such as asthma, diabetes, heart disease, kidney disease, high
blood pressure or other serious medical conditions.
What are the risks of this specific procedure +/- sedation?
There are risks and complications with this procedure. They include but are not limited to the following.
Common risks and complications include:
• Nausea and vomiting.
• Faintness or dizziness, especially when you start to move around.
• Headache.
• Pain, redness or bruising at the sedation injection site (usually in the hand or arm)
• Muscle aches and pains.
• Allergy to medications given at the time of the procedure
Uncommon risks and complications include:
• About 1 person in every 1,000 will experience bleeding from the esophagus (food pipe),
stomach and duodenum where a lesion or polyp were removed. This is usually stopped through the
endoscope. Rarely, surgery is needed to stop bleeding.
• Heart and lung problems such as heart attack or vomiting in the lungs causing pneumonia.
Emergency treatment may be necessary.
• Damage to your teeth or jaw due to the presence of instruments in your mouth.
• An existing medical condition that you may have got worse.
Rare risks and complications include:
• Missed polyps or growths.
• About 1 person in every 5,000 will accidentally get a hole (perforation) in the esophagus, stomach or
duodenum. This can cause a leak of stomach contents into the abdomen. If a hole is made, you will
be admitted to the hospital for further treatment which may include surgery.
• Your procedure may not be able to be finished due to problems inside your body or because of
technical problems.
• Bacteremia (infection in the blood). This will need antibiotics.
• Dead am’ type feeling in any nerve, due to positioning with the procedure - usually temporary.
• Anaphylaxis (severe allergy) to medication given at the time of the procedure.
• Death as a result of complications to this procedure is rare.
Your responsibilities before having this procedure
You are less at risk of problems if you do the following:
• Bring all your prescribed drugs, those drugs you buy over the counter, herbal remedies and
supplements and show your doctor what you are taking. Tell your doctor about any allergies or side
affects you may have.
• Do not drink any alcohol and stop recreational drugs 24 hours before the procedure. If you have a
drug habit, please tell your doctor.
• If you take Warfarin, Persantin, Clopidogrel (Plavix or Is cover), Asasantin or any other drug that is
used to thin your blood ask the doctor ordering the test if you should stop taking it before the
procedure as it may affect your blood clotting. Do not stop taking them without asking your doctor.
Tell your doctor if you have;
• had heart valve replacement surgery.
• received previous advice about taking antibiotics before a dental treatment or a surgical procedure.
If so, you may also need antibiotics before the colonoscopy.
Preparation for the Procedure
Your stomach must be empty for the procedure to be safe and thorough, 50 you will not be able to eat or drink anything for at least six hours before the procedure.
What if the doctor finds something wrong?
Your doctor may take a biopsy (a very small piece of the stomach lining) to be examined at Pathology.
• Biopsies are used to identify many conditions even if cancer is not thought to be the problem.
What are the polyps and why are they removed?
Polyps are fleshy growths in the bowel lining, and they can be as small as a tiny dot or up to several
centimeters in size. They are not usually cancer but can potentially grow into cancer over time. Taking
polyps out is an important way of preventing bowel cancer. The doctor usually removes a polyp along the
endoscope by using a wire loop. An electric current is sometimes also used. This is not painful.
What is I don’t have the procedure?
Your symptoms may become worse, and the doctor will not be able to give you the correct treatment
without knowing the cause of your problems.
Is there any other test I can have instead?
No. Your doctor could discuss with you other ways of managing your condition.
What can I expect after this procedure?
• You will remain in the recovery area for about 2 hours until the effect of the sedation wears of.
• Your doctor will tell you when you can eat and drink. Most times this is straight after the procedure.
• Your throat may feel sore and you might have some cramping pain or bloating because of the air
entering the stomach during the procedure.
• You will be told what was found during the examination or you may need to come back to discuss the
results, and to find out the results of any biopsies that may have been taken.
What is the safety issue?
Sedation will affect your judgment for about 24 hours. For your own safety and in some cases legally;
• Do NOT drive any type of car, bike or other vehicles. You must be taken home by a responsible adult
person.
• Do NOT operate machinery including cooking implements.
• Do NOT make important decisions or sign a legal document.
• Do NOT drink alcohol, take other mind-altering substances, or smoke. They may react with sedation
drugs
• Have an adult with you on the first night after your surgery.
Notify the hospital Emergency Department straight away if you have;
• severe ongoing abdominal pain.
• trouble swallowing.
• fever.
• Sharp chest or throat pain.
• have redness, tenderness or swelling for more than 48 hours where you had the injection for
sedation
(Either in the hand or arm).
What are my specific risks?
There may also be risks specific to your: Individual condition and circumstances, Please
discuss these with your doctor/healthcare professional and ensure they are written on the
consent form before you sign.
What are the risks of not having sedation?
There may be consequences if you choose not to have the sedation. Please discuss these with your
doctor/healthcare professional.
What are the responsibilities before having Sedation?
You are at least is of problems from anesthetic if you do the following. In preparation for your procedure:
• Increase your fitness before your procedure to improve your blood circulation and lung health ask
your doctor about exercising safely.
• If you are overweight, losing some weight will reduce many of the risks of having an anesthetic. Ask
your GP about losing weight safely.
• Stop smoking as early as possible before your surgery to give your lungs and heart a chance to
improve. Smoking cuts down the oxygen in your blood and increases breathing problems during and
after an operation
• Drink less alcohol as alcohol may alter the effect of the anesthetic medicines. Do not drink any
alcohol 24 hours before. surgery.
• Stop taking recreational drugs before your surgery as these may affect the anesthetic.
• If you take anticoagulant or antiplatelet (blood thinning) medicines, such as warfarin, aspirin,
clopidogrel (Plavix, is cover, Coplavix) prasugrel (Effient), dipyridamole (Persantin or Asasantin.
ticagrelor Brita) ticlopidine (Toldene) apixaban (Eliquis, dabigatran (Pradaxa), rivaroxaban (Xarelto)
or complementary /herbal /alternative medicines, such as fish oil or turmeric:
• If you are asked to stop taking blood thinning medicine before your procedure, ask your doctor when
you can restart the blood thinning medicine.
On the day of your procedure:
• Nothing to eat or drink (nil by mouth): you will be told when to have your last meal and drink. Do NOT
eat (including lollies) dink, or chew gum after this time otherwise your operation may be delayed or
cancelled. This is to make sure your stomach is empty so that if you vomit. There will be nothing to
go into your lungs.
• If you are a smoker or drink alcohol: do not smoke or drink alcohol.
• If you are taking medicines: most medicines should be continued before an operation but there are
some important exceptions:
• your doctor will provide specific instructions about your medicines.
• take to the hospital all your prescribed medicines those medicines you buy over the counter, herbal
remedies and supplements to show your anesthetist what you are taking.
• If you feel unwell telephone the ward/ hospital for advice.
• Tell your doctor and the anesthetist f you have:
• health problems (e.g., diabetes, high blood pressure, infectious diseases, serious illnesses),
including if regular treatment or a stay in the hospital is needed.
• an alcohol or drug addiction.
• had previous problems and/or known family problems with anesthesia.
• false teeth, caps, loose teeth or other dental problems.
• any implants you have.
• been taking prescribed and/or over-the-counter medicines, herbal remedies and supplements this
may include and are not limited to blood-thinning medicines. the contraceptive pill, antidepressants
and/or diabetic medicines (e.g., insulin).
• allergies/ intolerances of any type and side effects.
• ask your surgeon and/ or anesthetist if you should stop taking it before surgery as it may affect your
blood clotting.
• Do NOT stop blood thinning medicines without asking your doctor.
What happen after the procedure has finish?
After the procedure, the nursing staff will watch you closely until you are fully awake This is usually in
an area known as recovery. You will then be given something to eat and drink. You can rest until you
have recovered enough to home.
Follow Sedation:
Sedation medicines may affect your judgment for about 24 hours or sometimes longer. For your own safety
during this time:
• Ask your doctor/ health professional whether you can:
• drive any type of car, bike or their vehicle.
• operate machinery including cooking implements.
• Do NOT important decisions (such as withdrawal of money from the ATM machine) or sign legal
documents.
• Do NOT drink alcohol, take other mind-altering substances, or smoke as these substances
• may react with the sedation medicines.
• Have an adult with you on the first night after your procedure.
Patient Information, Terms and Conditions
The Intra-Gastric Balloon procedures (hereinafter referred to as gastric balloon or the procedure) offer a
simple, safe, and effective method for combating obesity. Their role in helping patients to lose weight and
maintain that weight loss is proven. However, it's vitally important to understand that gastric balloons are
medical devices being used in a medical context. It is not a toy or a gimmick that will do all the work for you.
Consequently, we would ask that you read and understand the following.
Regarding the Procedure - You understand that:
The procedure s an elective procedure, requested by you, you have been consulted by the staff of the
and you have had every opportunity to discuss the procedure. That the pros and cons
and risks and complications of the procedure will be discussed with you by your Endoscopic and Endo
Bariatric Surgeon
procedure will be undertaken by Endoscopic and Endo-Bariatric Surgeon,The procedure will almost always require sedation anesthesia which will be administered by the Specialist
Anesthetist.
That the procedure may rarely require general anesthesia which will be administered by a Specialist
Anesthetist in one of our partner hospitals.
That the procedure is carried out on a day case basis but may rarely require an overnight stay which is not
included in your package in one of our partner hospitals.
That there are potential risks and complications with any section and/or general anesthesia and that these
are to be discussed with the Surgeon and Anesthetist,
However, notwithstanding any subsequent discussions with doctors, you accept and understand that these
complications include but are not limited to the following:
• Adverse reactions to the anesthetic drugs or any other medications that may have to be administered
• Damage 10 teeth
• Sore throat
• Damage to the vocal cords
• Heart complications, including cardiac arrest
• Lung complications. including aspiration of stomach contents, chest infection, pulmonary embolism
• Thromboembolism
• Hyperpyrexia.
• Death
You confirm that you understand these anesthetic complications to be extremely rare in an otherwise fit and
healthy patient undergoing routine non-urgent sedation.
You also confirm that if any complications happen you may be transferred to one of our partner hospitals
and given under the care of the medical team in that hospital setting If needed.
You understand that:
The procedure itself involves passing an endoscope through the mouth, down the gullet, and into the
stomach, where a thorough examination will be undertaken prior to insertion of the gastric balloon
There are potential risks and complications with any endoscopic examination and that these are to be
discussed with the Endoscopic Surgeon. However, notwithstanding any subsequent discussions with the
Endoscopic Surgeon.
You accept and understand that these complications include but are not limited to the following:
• Abdominal discomfort because of the air pumped into the stomach to distend it
• Injury to the gullet or stomach (including perforation - even very rare)
• That any such injury may result in bleeding and/or perforation.
• That any such injury may require further emergency surgery and that you specifically consent to any
such emergency surgery.
• Inhalation/ aspiration of gastric contents (even very rare)
You understand that:
If any abnormality is found during the examination, the procedure may have to be abandoned, perhaps
permanently.
Following the examination, the gastric balloon will be passed through the mouth down the gullet and into
the stomach where its position will be confirmed endoscopically, and then it is inflated with sterile saline in
which there is a blue dye.
That there are potential immediate risks and complications associated with the insertion of the intragastric
balloon and that these are to be discussed with the Endoscopic Surgeon.
However, notwithstanding any subsequent discussions with the Endoscopic Surgeon. you accept and
understand that these complications include but are not limited to the following:
• Injury to the gullet or stomach including perforation - even very rare).
• Bleeding due to trauma (even very rare)
Rupture of the gullet or stomach on inflation of the intragastric balloon (even very rare).
You understand that:
Medications. Other treatment and/or surgery may be necessary during the course of the procedure should
any complications arise, and you specifically consent to these also.
Even once the gastric balloon is successfully inserted, other complications may arise, and that these are to
be discussed. with the Endoscopic Surgeon and Specialist Anesthetist. However, notwithstanding any
subsequent discussions with the Endoscopic Surgeon and Specialist Anesthetist, you accept and
understand that these complications include but are not limited to the following:
• Balloon intolerance.
• Dehydration dL to prolonged sickness may require IV fluids at our clinic during day time or your
closest hospital.
• Metabolic problems +/- renal failure/thiamine deficiency.
• Reflux esophagitis.
• Gastric erosions +/- bleeding.
• Gastric ulcers +/- a perforation.
• Gas outlet obstruction/balloon impaction.
• Acute gastric dilatation.
• Balloon deflation.
• Spontaneous evacuation of the balloon at stool.
• Intestinal obstruction.
• Infections.
• Alterations in bowel habits,
You understand that if any complications do arise, you will contact the or any
emergency services of our hour service immediately and accept their advice regarding care. If you need to
be moved to a hospital for care, costs are not included in the Enfield Royal Wellness Management
packages.
Your package does not include any other hospital treatment or accommodation which will be charged
separately by a related hospital.
Regarding Weight Loss,
The gastric balloon is an accepted method of treatment for mild to moderate obesity in adults. This
procedure is being undertaken to help you control your weight.
In recorded discussions with the , you have confirmed that you have a history of obesity
and a poor relationship with food. and that you have tried alternative forms of treatment over years and all
have been unsuccessful, and all other treatment modalities have been discussed with you including general
dietary control. very low-calorie diets, anti-obesity medications, and anti-obesity surgery. After all these
discussions
relating to alternative treatment modalities, we have agreed that the very best course of treatment for you is
the gastric balloon.
You understand that:
The gastric balloon is a training tool to help with behavior modification and that you must participate in
dedicated follow-ups for behavioral modification and support to increase its chance of success.
Consequently, you will do all that you can to help yourself in this process, including attending all review
appointments in person, by telephone or by internet calls.
You have been advised that, following the removal of the intragastric balloon, further follow-ups and other
consultations of behavioral modification and further care may be required and that you will attend all
appointments for this, and follow all advice given to you.
No specific assurance has been given to you about the amount of weight that you may lose.
The gastric balloon must be removed within a period of six or twelve months depending on which balloon
you chose and you hereby also consent to its removal at that time.
Regarding Unforeseeable Circumstances
An Abnormality Found at Endoscopy - You understand that:
If during your endoscopy an abnormality is found. it may not be possible to insert the gastric balloon,
temporarily or permanently.
If following endoscopy, it is not possible to insert your gastric balloon at all. including at any time in the
future:
• You will receive a refund of any monies remaining after all incurred costs have been deducted costs
will include but are not limited to: Doctors’ consultations, body composition analysis, blood tests, and
cost of the upper gastrointestinal endoscopy (Gastroscopy),
If following endoscopy. you are found to have a treatable benign condition that merely means your balloon
placement must be postponed, the decision as to whether to be treated and then proceed is entirely yours.
• If you decide to proceed, you understand that costs have already been incurred and there will be
additional upper gastrointestinal endoscopy (Gastroscopy) and other procedures such as biopsy, if
any, cost to pay.
Failure To Follow Eating/Fasting instructions –
You understand that:
Failure to follow pre-insertion eating and fasting instructions may result in your procedure being
abandoned.
If food is found in your stomach and it is not possible to insert the intragastric balloon:
• Should you decide to proceed at a later date you understand that costs have already been incurred
and there will be additional Upper gastrointestinal endoscopy (Gastroscopy) cost to pay.
• If you decide not to reschedule you will receive a refund of any monies remaining after all incurred
costs have been deducted. Costs will include but are not limited to: Doctors consultations, body
composition analysis, blood tests, and the cost of the upper gastrointestinal endoscopy
(Gastroscopy).
Balloon Intolerance
If you have a genuine intolerance extremely your balloon will be removed immediately. No refund will be
given
as all costs have been incurred
If you choose to have your balloon removed early for whatever reason, no refund will be given.
If you choose not to complete or participate in the Weight Management Unit Programme at Enfield Royal
Clinic for any
reason including following the early removal of your balloon, no refund will be given.
As reported by the manufacturers of gastric balloons, the early balloon removal rate due to intolerance is
around 7%
Spontaneous Balloon Deflation/ Intestinal Obstruction - You understand that:
Spontaneous balloon deflation is an unusual event in patients who take all their prescribed medication and
who attend for balloon removal within the stated six months. If you suffer from this complication, you may
notice your urine and/or stools change the colour of blue:
• You must immediately contact the Weight Management Unit and/or the closest
hospital emergency service. The balloon will be removed endoscopically if. as is almost certainly the
case, the balloon is still in the stomach
• If you do not contact us or any emergency services immediately and/or the balloon has already of the
stomach, it may cause a life treating health situation. In this situation, your progress will be monitored
closely and may require hospital admission. x-rays or other investigations and surgical or non
surgical treatments will not be covered in your packages.
Failure to lose Weight
With any medical procedure or biological process there is a range of success recorded. Some patients
must naturally do better than others, some may even cheat and continue to eat or drink very high-calorie
liquidized food. The ‘ Care Weight Management Unit Programs are specifically set up to
maximize a patient's own potential for success. We are therefore unable to offer any refund whatsoever in
the event that patients are disappointed with the results of their gastric balloon,
Important Note
The Weight Management Unit insists that the gastric balloon be removed within the
stated six-month period. If you fail to attend for balloon removal at this time, any and all complications that
ensue thereafter will be at your own risk and your own expense.
It is not always possible to return to the same hospital for the removal of your balloon. Occasionally, due to
unforeseen circumstances. you may be booked into another hospital for the removal procedure.
Weight management unit Intra-Gastric Balloon by upper Gastrointestinal Endoscopy (Gastroscopy) Assistance for weight loss
Informed Consent Form
I have read and understood the contents of GASTROSCOPY, SEDATION ANESTHESIA and INTRAGASTRIC BALLOON INFORMATION including the risks and possible complications before, during, and after these procedures. The procedures and their associated risks and possible complications have been clearly explained to me, | had the opportunity prior to the procedures to direct all my questions to the attending doctor and were given satisfactory answers.
I am not breastfeeding:
I am not pregnant and do not think | may be pregnant during my 6-month programmed:
I, hereby give my consent to doctors of to perform a Gastroscopy (with or without biopsy/polypectomy) and Intragastric Balloon Placement on me
I understand and agree that I am financially responsible for the payment I made for that any amount I paid for the sessions or procedures I booked it will only be valid up to 3 months from the date I made the payment. I understand that I need to utilize the sessions or procedures within 3 months period. I agree that my payment made is non-refundable or non-transferable post this period.
I declare that I have read and fully understood all points in this consent and that all of my questions were answered to my satisfaction and I take the full responsibility of my decision in this consent.



I, , consent to be photographed and published on Social media, by while before and after the procedure. I further authorize that the photographs may be published for any purpose and in any form.
